Tooth infections can be more than just a painful inconvenience. They can escalate quickly, transforming from a minor annoyance into a serious health threat. You might think of toothaches as simple dental issues that require little attention, but the reality is quite different. If left untreated, these seemingly harmless infections can lead to life-threatening complications.
Many people underestimate how quickly an infection in the mouth can spread throughout the body. Understanding the timeline and risks involved is crucial for your health and well-being. So how long until a tooth infection kills you? The answer may surprise you.
In this blog post, we’ll explore what happens when a tooth infection occurs, its symptoms and causes, diagnosis methods used by professionals, management strategies for treatment, preventive measures you should take seriously—and ultimately what outlook to expect if one finds themselves grappling with an oral infection. Stay informed how long until a tooth infection kills you; your smile depends on it!
Overview How Long Until A Tooth Infection Kills You
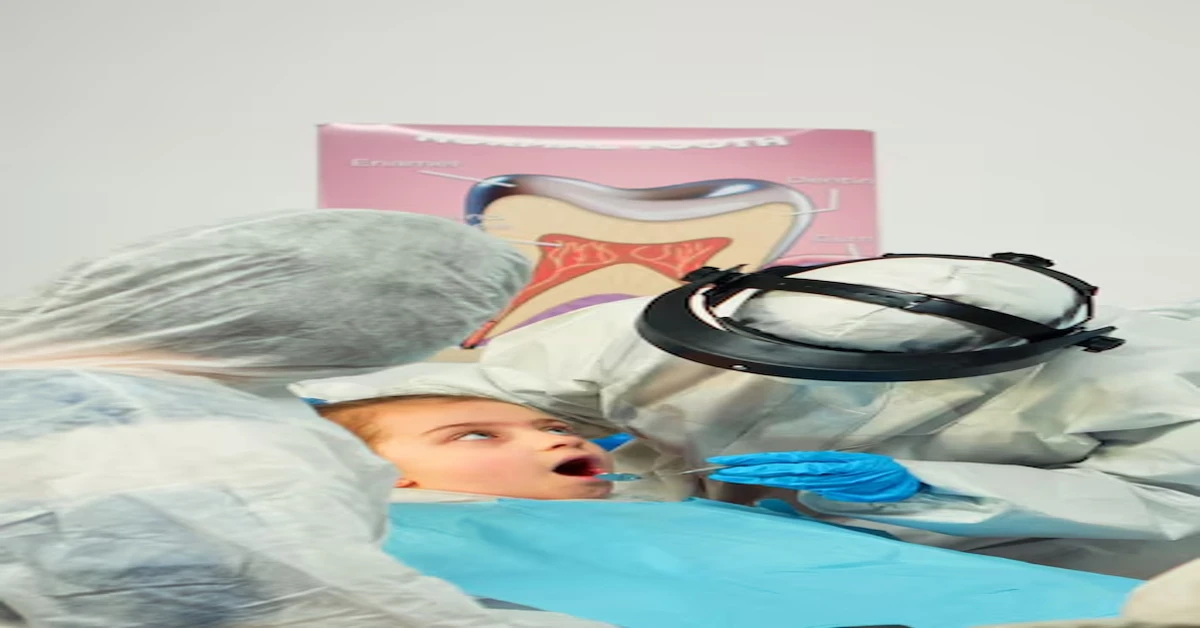
Tooth infections, also known as dental abscesses, arise when bacteria infiltrate the inner layers of a tooth. They often start with untreated cavities or gum disease and can quickly progress if not addressed promptly.
Once bacteria enter the pulp—the soft tissue inside your tooth—they begin to multiply rapidly. This leads to inflammation and pain, creating an environment ripe for infection. The body responds by sending white blood cells to fight off the invaders, resulting in pus accumulation.
Infections can spread beyond the tooth itself, affecting surrounding tissues and even entering the bloodstream. This is where things become particularly dangerous. What may have started as a localized issue can turn into a systemic problem requiring urgent care.
The speed at which this escalation occurs varies from person to person. Factors like overall health, immune response, and promptness in seeking treatment play significant roles in determining how fast an infection can become life-threatening.
Ignoring symptoms—such as persistent pain, swelling around the gums or face, fever, or difficulty swallowing—can lead to dire consequences. It’s easy to dismiss these signs until they result in serious complications that could affect vital organs like your heart or brain.
Understanding these risks underscores why timely intervention is crucial for managing dental health effectively. Awareness of what constitutes a severe infection empowers individuals to take action before it’s too late.
So while many view tooth infections as trivial issues best suited for later attention—this perspective could prove fatal over time without proper vigilance so know about how long until a tooth infection kills you.
Symptoms and Causes
Tooth infections can manifest in various ways, often presenting symptoms that are hard to ignore. The initial signs might include a persistent toothache that worsens over time. This pain is usually localized but can radiate to the jaw or even the ear.
Swelling around the affected area is another common symptom. As pressure builds from infection and inflammation, you may notice your gums becoming puffy and red. This swelling can also extend to your face, making it look lopsided or swollen.
Fever often accompanies a tooth infection as your body fights off bacteria. A low-grade fever may be manageable, but if it spikes higher than usual, it’s an urgent sign that intervention is needed.
In some cases, you could experience difficulty swallowing or breathing due to swelling obstructing airways or esophageal pathways. These symptoms should never be ignored; they signal severe complications and how long until a tooth infection kills you.
Bad breath or an unpleasant taste in your mouth frequently indicates pus buildup from an abscessed tooth. It’s not just annoying; these odors reveal bacterial activity that’s wreaking havoc inside your mouth.
The causes of tooth infections typically stem from dental issues like decay or gum disease. Bacteria enter through cavities or cracks in teeth, establishing a foothold where they multiply rapidly.
Trauma to the teeth—whether from accidents or grinding—can also invite trouble by creating openings for bacteria to invade deeper tissues surrounding the roots and jawbone.
Diagnosis and Tests
When you suspect a tooth infection, seeking prompt medical attention is crucial. The right diagnosis can make all the difference in preventing serious complications.
Your dentist will begin with a thorough examination of your mouth. They’ll look for visible signs of infection, such as swelling, redness, or pus around the affected tooth. This initial inspection helps identify potential problem areas.
Next comes imaging studies, often in the form of X-rays. These images provide insight into the extent of the infection and whether it has spread to surrounding tissues or even bones. X-rays are an invaluable tool; they can reveal hidden issues that aren’t immediately apparent during an exam.
In some cases, further tests may be necessary to determine if bacteria have entered your bloodstream. Blood tests can help assess overall health and detect any systemic infections that could arise from dental issues.
If you’re experiencing severe symptoms like fever or difficulty swallowing, your healthcare provider might recommend additional evaluations to rule out complications like abscesses or sepsis.
Your dental professional will also ask about your symptoms and any previous history related to oral health problems. It’s essential to share details honestly; this information plays a vital role in determining how urgently treatment is needed.
Remember that timely diagnosis not only alleviates discomfort but also safeguards against potentially life-threatening outcomes associated with untreated infections.
Management and Treatment
When it comes to managing a tooth infection, prompt action is crucial. The first step often involves visiting your dentist or healthcare provider as soon as possible. They will assess the severity of the infection and determine how long until a tooth infection kills you suggesting an appropriate treatment plan tailored just for you.
Antibiotics are usually prescribed to fight bacterial infections. These medications can help reduce inflammation and eliminate bacteria from the infected area. It’s important to take them exactly as directed by your healthcare professional.
In some cases, draining the abscess may be necessary. This procedure allows pus accumulation to escape and relieves pressure in the affected area. Your dentist may perform this simple yet effective procedure during your visit.
Pain management plays a significant role in treating tooth infections too. Over-the-counter pain relievers like ibuprofen or acetaminophen can provide relief while waiting for further treatment options. Always follow dosage instructions carefully.
If antibiotics alone do not resolve the issue, more invasive treatments might be required. Root canal therapy could become necessary if the infection has reached deeper structures within the tooth itself.
In severe instances where extensive damage has occurred how long until a tooth infection kills you, extraction of the affected tooth may be needed to prevent further complications. While it sounds daunting, sometimes this is essential for safeguarding overall health.
After treatment, maintaining good oral hygiene is vital for recovery and prevention of future infections. Regular dental check-ups will ensure any issues are caught early on before they develop into something more serious.
Prevention
Preventing a tooth infection is easier than most people think. It begins with good oral hygiene. Brushing your teeth twice daily, using fluoride toothpaste, can significantly reduce the risk of cavities and gum disease.
Flossing should not be overlooked. Regularly cleaning between your teeth removes food particles and plaque that brushing alone might miss. This simple act is crucial for maintaining healthy gums.
Routine dental check-ups are essential too. Seeing your dentist at least twice a year allows for early detection of potential issues before they escalate into serious problems. Your dentist can provide professional cleanings that further protect against how long until a tooth infection kills you.
Diet plays a pivotal role in prevention as well. Consuming a balanced diet rich in vitamins and minerals supports strong teeth and gums. Limiting sugar intake reduces the chances of cavity development, which can lead to infections.
If you have existing dental issues like cracked or decayed teeth, addressing them promptly is vital. Ignoring these problems increases the risk of bacteria entering deeper tissues, heightening the likelihood of an infection forming.
Avoid smoking or chewing tobacco products as these habits significantly impair oral health by reducing blood flow to the gums and increasing bacterial growth around teeth.
Stay hydrated! Drinking plenty of water helps wash away food particles and keeps saliva levels high—saliva acts as your mouth’s natural defense system against harmful bacteria.
Outlook / Prognosis
Tooth infections can escalate into serious health concerns if left untreated. The timeline for a tooth infection to become life-threatening varies based on several factors, including the individual’s overall health and how quickly they seek medical attention.
When treated promptly, most people recover fully from dental infections. Antibiotics and proper dental care often clear up the issue without complications. However, neglecting symptoms or delaying treatment can result in severe consequences. Infections may spread to other parts of the body, leading to conditions like sepsis or affecting vital organs.
For those with pre-existing health issues—such as diabetes or compromised immune systems—the risks increase significantly. These individuals should be especially vigilant about oral hygiene and any signs of infection. Regular check-ups with a dentist are crucial for early detection and intervention.
The prognosis is generally positive when addressed early on. Being proactive about symptoms and seeking immediate care can mean the difference between a simple procedure and more extensive treatment needs later on.
Maintaining good oral hygiene practices not only helps prevent tooth infections but also ensures your overall well-being remains intact. Remember that timely action is key; don’t let a small problem turn into something far worse than it ever had to be.